Diabetic Neuropathy Device™
One Device. Two Fibers. Zero Guesswork.
Diabetic Peripheral Neuropathy
Diabetic Neuropathy is often silent—until it’s too late. The Diabetic Neuropathy Device™ (DND) changes that by offering the only FDA-registered solution that objectively assesses both small and large fiber nerve function at the point of care.
Unlike subjective pinprick tests or tuning forks, the DND delivers quantifiable data in 3-minutes or less—enabling early detection, documented medical necessity, and multi-visit therapy planning

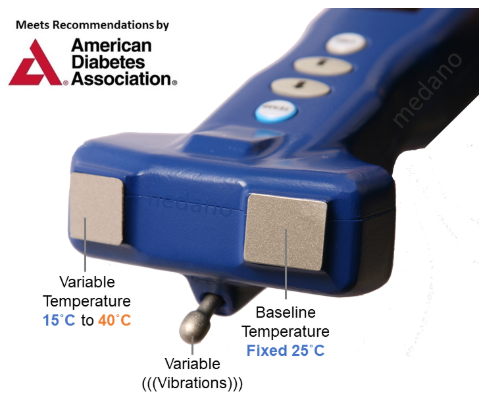
Temperature (Small Fiber)
The Device (DND) Replaces Tuning Forks and Monofilaments...
Kazu Suzuki DPM, Medical Director of the Tower Wound Care Center at the Cedars-Sinai Medical Towers in Los Angeles, CA; Managing Neuropathy And Pain In Wound Care Patients, Podiatry Today; September 2015; 26-27.

Site-Specific Predictive Biomarkers

Vibration (Large Fiber)
“Every medical practice should test patients with the DND before referring them to a specialist because it can help identify potential underlying conditions that may require further investigation or treatments.” –J. Gonzalez MD, Neurologist
Comprehensive Foot Exams (Painful/Painless)
Get Reimbursed for Foot Exams
Monofilament testing, although affordable and widely used, is not without limitations. The perception that inexpensive tools like monofilaments are sufficient for diagnosing neuropathy can lead to delayed interventions and an increased risk of complications. A study published in the Journal of Diabetes Science and Technology highlighted that monofilaments have a sensitivity of only 64% for detecting diabetic peripheral neuropathy, raising concerns about their reliability. This underscores the need for more accurate and objective diagnostic methods to ensure early detection and better patient outcomes. Relying on subjective and outdated tools such as monofilaments or tuning forks risks false negatives that delay critical care and false positives that lead to unnecessary interventions. Medical providers must consider modern alternatives that improve diagnostic accuracy and qualify for reimbursements, ensuring better care and financial viability for clinics.
Diabetic and Non-Diabetic
The Diabetic Neuropathy Device™ (DND), introduced in 2014, represents a significant advancement in detecting and measuring neuropathy. Clinical studies demonstrate that the DND provides more precise and reliable results than traditional tools like monofilaments and tuning forks, which are prone to false positives and negatives.
With the DND, medical providers can standardize diabetic foot exams across the United States, ensuring consistent and effective patient care. This groundbreaking tool enables accurate diagnosis and monitoring of diabetic neuropathy, leading to timely treatments and improved outcomes. Recognized as the most significant innovation in diabetic neuropathy detection in over 80 years, the DND is a clinical necessity and eligible for reimbursement from Medicare, Medicaid, and commercial insurers.
Investing in the DND is an investment in better patient outcomes, reduced complications, and a modernized approach to neuropathy care. By adopting this innovative device, providers can elevate their standard of care and ensure that patients receive the best possible management for diabetic and non-diabetic neuropathy.
Diabetic Neuropathy Accounts for More Hospitalizations Than All Other Diabetic Complications Combined...
Aaron Vinik, MD, Ph.D., Endocrinologist, Diabetic Neuropathies, February 5, 2018
“The DND has improved the patient understanding of their disease, which is very helpful.” – W. Beaton DPM
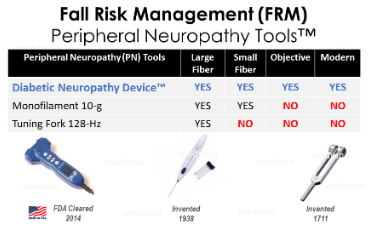
Bild DE, et al. Lower Extremity Amputations in People with Diabetes: Epidemiology and Prevention. Diabetes Care 1989; 12:24-31; CDC MMWR November 01, 1991 / 40(43);737-7
What Makes it Different:
- Dual-Fiber Detection: Detects both small (unmyelinated) and large (myelinated) nerve damage—critical for diabetic and prediabetic patients
Fully Objective & Non-Invasive: No guesswork, no pain—just reproducible results providers can trust
Medicare-Reimbursable Valid CPT codes supported by strong clinical documentation
Testing in 3 Minutes or Less Fits into your existing workflow without disrupting patient volume
Supports Amputation Prevention Protocols Ideal for patients with diabetes, PAD, or CKD—before symptoms become irreversible
“We regularly use the Diabetic Neuropathy Device™ (DND) to monitor our diabetic patients who are at risk for developing diabetic neuropathy, as well as patients who are already diagnosed with diabetic neuropathy.” -C. Soller NP, Endocrinology
Modern Technology
The Diabetic Neuropathy Device™ (DND) aligns with the latest screening and diagnostic recommendations from the American Diabetes Association (ADA). As the only tool capable of screening for distal symmetric polyneuropathy (DSPN) by assessing both temperature sensitivity (small fiber function) and vibration perception (large fiber function), the DND sets a new standard in neuropathy diagnostics, as emphasized in the ADA’s Diabetic Neuropathy: A Position Statement by the American Diabetes Association.
Tailored neuropathy treatments are essential to address each patient’s unique clinical presentation and underlying pathology while avoiding the risks associated with opioid use. For example, treating painful neuropathy with pain-relieving medications alone may mask loss of protective sensation (LOPS) in the feet, leaving patients vulnerable to foot ulcers and amputation. Early and accurate identification of neuropathy allows providers to intervene at the earliest stages of the condition, effectively reducing risk factors and improving outcomes.
By leveraging advanced tools like the DND, medical providers can enhance their ability to diagnose, monitor, and manage diabetic neuropathy, ultimately protecting patients from severe complications and improving their quality of life.
Don't Change Your Workflow, Just Your Tools!
Boris Golosarsky, MD MACP FACPI, Podiatry Management, Profiles in Excellence, January 2015
The DND objectively measures both small and large fiber neuropathy—enabling earlier detection, full nerve assessment, and more comprehensive diagnostics in one device.
“We use the DND because it gives us both the small and large fiber results that we feel are important for every diabetic patient.” –R. Cardenas MD, Family Practice
Importance of Specificity
Neuropathy is a serious condition that, if not accurately diagnosed and treated promptly, can lead to devastating outcomes, such as amputations of the toes, feet, or legs. The failure to adopt advanced diagnostic tools and procedures has resulted in medical institutions and physicians being held liable for malpractice. A landmark case, Washington v. Washington Hospital (1990)., set legal precedent in the U.S. regarding this issue.
To mitigate these risks, clinicians must stay informed about emerging best practices that are supported by clinical evidence. By adopting advanced technologies and emphasizing prevention, healthcare providers can improve patient outcomes while reducing the risk of complications. Proactive strategies, such as reallocating resources toward early detection and intervention, enable the administration of appropriate therapies. This approach can ultimately decrease the need for frequent inpatient and outpatient visits, significantly enhancing patients’ quality of life.
"...by the time a patient fails the monofilament test, he or she may have a profoundly severe neuropathy, and it may be too late to intervene."
Kazu Suzuki DPM, Medical Director of the Tower Wound Care Center at the Cedars-Sinai Medical Towers in Los Angeles, CA; Managing Neuropathy And Pain In Wound Care Patients, Podiatry Today; September 2015; 26-27.
Aaron Vinik, MD, PhD, FCP, MACP, FACE, et al, Endocrinologist, Diabetic Neuropathies, February 5, 2018

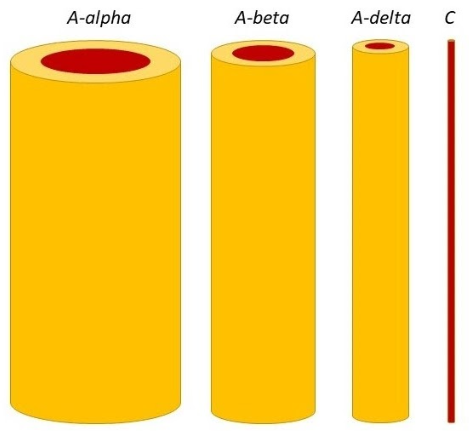
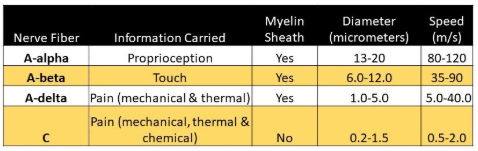
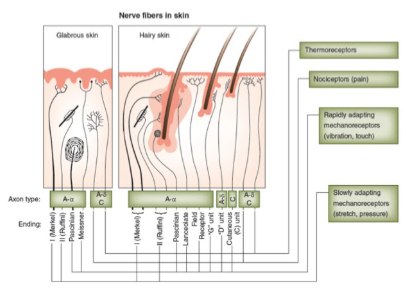
Identifying the following nerve fibers may increase earlier awareness and interventions:
Aα fibers are large myelinated fibers in charge of motor functions and muscle control.
Aβ fibers are large myelinated fibers with sensory functions such as perception to touch, vibration, and position.
Aδ fibers are small myelinated fibers in charge of pain stimuli and cold perception.
C fibers can be myelinated or unmyelinated and have sensory (warm perception and pain) and autonomic functions (blood pressure and heart rate regulation, sweating, etc.).
“One of the great advantages of using the DND on our diabetic patients who have started to develop diabetic neuropathy, is that showing them their results, often makes the consequences of not taking care of themselves more realistic.” -S. Erle DC, Neuropathy Centers
Morbidity and Mortalities
Diabeticsthat have lower-extremity amputations have lifespans that range between 40% mortality in 1-year, 65% mortality in 3-years, and 80% mortality in 5-years. Diabetic Neuropathy is a serious diabetes complication affecting as many as 50% of people who suffer from pain, and another 50% may be asymptomatic – who are at the highest risk of falls, ulcerations, and amputations. Nerve damage and poor circulation are the most common causes of diabetic foot problems. One of the most underdiagnosed and untreated parts of a comprehensive foot exam is checking the loss of protective sensation (LOPS) in the feet. The diabetic large nerve fiber dysfunction, as measured by vibration, predicts foot ulcerations, amputations, and mortality.
(Painless) Diabetic large nerve fiber dysfunction as measured by vibration Predicts foot ulceration, amputation and mortality.
https://care.diabetesjournals.org/content/32/10/1896
The purpose of a comprehensive diabetic foot exam is to gather as much clinical data about the condition of a person’s normal or abnormal condition in the feet of both large and small nerve fibers. A diabetic foot exam also checks people with diabetes for infection, injury, and bone abnormalities. However, over 99% of all medical providers use outdated and subjective tools (tuning fork, invented in 1711 or monofilaments, invented in 1938) to identify a progressive disease. Distal Symmetric Polyneuropathy (DSPN), a glove and stocking distribution, is the most common form of Diabetic Neuropathy (DN) and is recognized as the most troublesome complication of diabetes mellitus leading to the greatest morbidity and mortality, which accounts for the most amount of hospitalizations than all other diabetic complications combined and is responsible for up to 75% of non-traumatic amputations.
Painful) Diabetic small fiber neuropathy can only be verified with thermal thresholds or skin biopsies.
Aaron Vinik, MD, Ph.D., Endocrinologist, Diabetic Neuropathies, February 5, 2018
The proper diagnosis of diabetic neuropathy should require tools to identify and measure the disorder quantitatively for the different abnormalities that occur to specific nerve fibers. Combining at least two different examinations (large and small fiber) will increase the sensitivity and specificity of detecting DPN. Currently, many medical providers are unaware of reimbursable tools that address both large fiber and small fiber neuropathy, both of which manifest in patients with diabetes. The Diabetic Neuropathy Device™ is the first FDA Cleared multi-objective tool with 15 measurements that identify both large and small nerve fibers in the upper and lower extremities.
Aaron Vinik, MD, PhD, FCP, MACP, FACE, et al, Endocrinologist, Diabetic Neuropathies, February 5, 2018
Mechanism of Action
The sympathetic skin response is a simple, reproducible, and non-invasive test based on modifying the skin potential of peripheral nerves. Sympathetic skin response has been used to diagnose polyneuropathy, erectile dysfunction, central degenerative diseases, multiple sclerosis, brain infarction, reflex sympathetic dystrophies, spinal, and peripheral nerve lesions. The Diabetic Neuropathy Device™ is a modern tool that uses the SSR to help patients discriminate against variable temperature and vibration stimuli.
Quantitative Sensory Testing (QST) and Sympathetic Skin Response tests (SSR) are distinct diagnostic procedures employed to assess the nervous system: QST focuses on evaluating sensory function by measuring the perception of stimuli, including touch, temperature, and pressure, commonly used in neurology to assess peripheral neuropathy; whereas SSR assesses the sympathetic nervous system’s activity by measuring changes in skin conductance in response to stress or stimuli, often applied in neurology to evaluate autonomic nervous system function, with key differences lying in their respective focuses, stimuli application methods, and measurements. Multiple studies have proven the value of Quantitative Sensory Testing (QST) measures in the detection of subclinical neuropathy (small fiber neuropathy), the assessment of the progression of neuropathy, and the prediction of the risk of foot ulceration (117,129,130). These standardized measures of vibration and thermal thresholds also play an important role as primary efficacy endpoints in multicenter clinical trials.





